Researchers have developed a protocol for studying how drug carrying nanoparticles called cubosomes behave in the body. The results show nanoparticle stability and confirm localisation in the cell. The study represents a significant step forward in the development of novel pharmaceuticals.
Drug carrier nanoparticles are used when the drug molecules, for example, are not stable enough to be transported on their own in the body, or to decrease side effects by more efficiently guiding the molecules to the intended target.
“Cubosomes are promising carriers for treating a range of diseases, particularly those requiring targeted drug delivery and controlled release. These include cancer, infectious diseases such as tuberculosis or fungal infections, inflammatory conditions, and neurological disorders. The cubosomes’ ability to deliver poorly soluble drugs and to be engineered for stimuli-responsive release makes them especially beneficial in cancer therapy, where they can enhance drug accumulation in tumours while minimizing off-target effects, says Iris Ribeiro from the Brazilian Center for Research in Energy and Materials (CNPEM), and one of the authors of the study.
The cubosomes consist of lipids, a type of molecule found in the body, that have arranged themselves into a cluster with pockets where the drug molecules can be stored during transport.
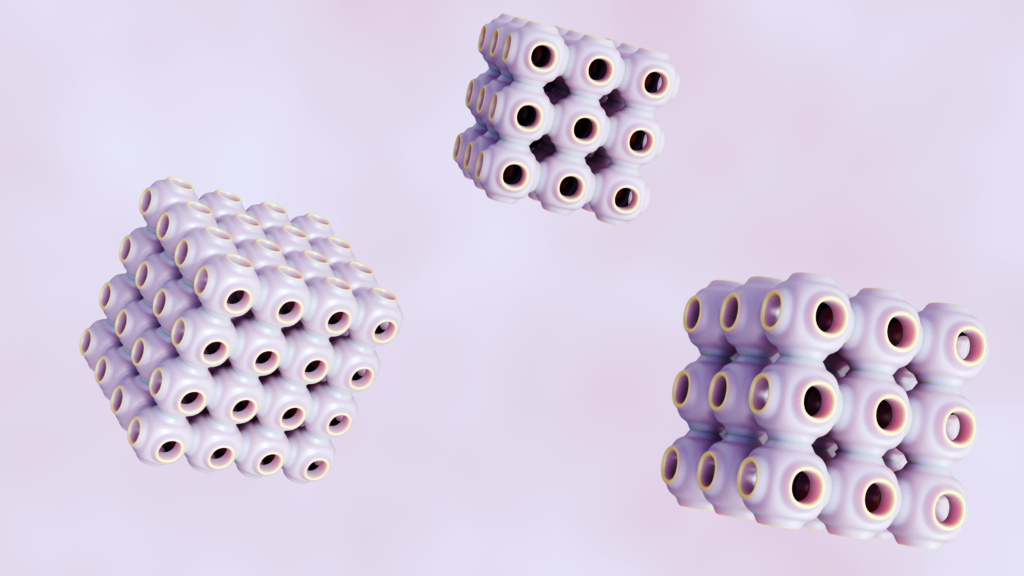
“The term cubosome was described for the first time in 1989. Interest in their use for biomedical applications, particularly in drug delivery, has increased significantly over the past two decades. Their biocompatibility, structural versatility, and ability to encapsulate both hydrophilic and hydrophobic drugs have made them a prominent subject of research in the nanomedicine field,” says Ribeiro.
The researchers studied how well the cubosomes are preserved when they are placed in a liquid like that which is present in cells. It is, for example, important that they don’t clump together in aggregates as cell toxicity depends on nanoparticle size. The team also used electron microscopy and X-ray methods to investigate where the cubosomes end up in the cell. They found that it is typically inside lysosomes, a part of the cell responsible for decomposition.
At MAX IV, the cubosomes were investigated by Small Angle X-ray Scattering (SAXS), at the CoSAXS beamline. SAXS is a technique that can say something about the shape and size of the particles. It was used to confirm the structure of the cubosomes after the drugs had been loaded, and it showed that they stayed essentially the same. If the cubosomes would change size or shape, they could become less effective.
The researchers confirm that they can measure the important parameters of the cubosomes using the protocol they have developed. They also investigated cell toxicity in breast cancer and normal cells at different concentrations of drug-loaded cubosomes, as well as for the empty cubosomes. When empty, the nanoparticles are not toxic to cells at specific concentrations, reinforcing that toxicity is concentration-dependent. One of the tested cubosome types also showed good performance in terms of low toxicity and high specificity to cancer cells when loaded with a cancer-fighting drug molecule.
“The next step in our research is to investigate drug delivery and nanoparticle internalisation in more physiologically relevant models, such as 3D cell cultures. Unlike traditional 2D monolayers, 3D models better mimic the architecture and complexity of real tissues, including gradients of oxygen and nutrients. Studying the cubosomes’ behaviour in these systems will provide deeper insights into their therapeutic performance and help bridge the gap between studies on model systems and real-life applications,” says Ribeiro.